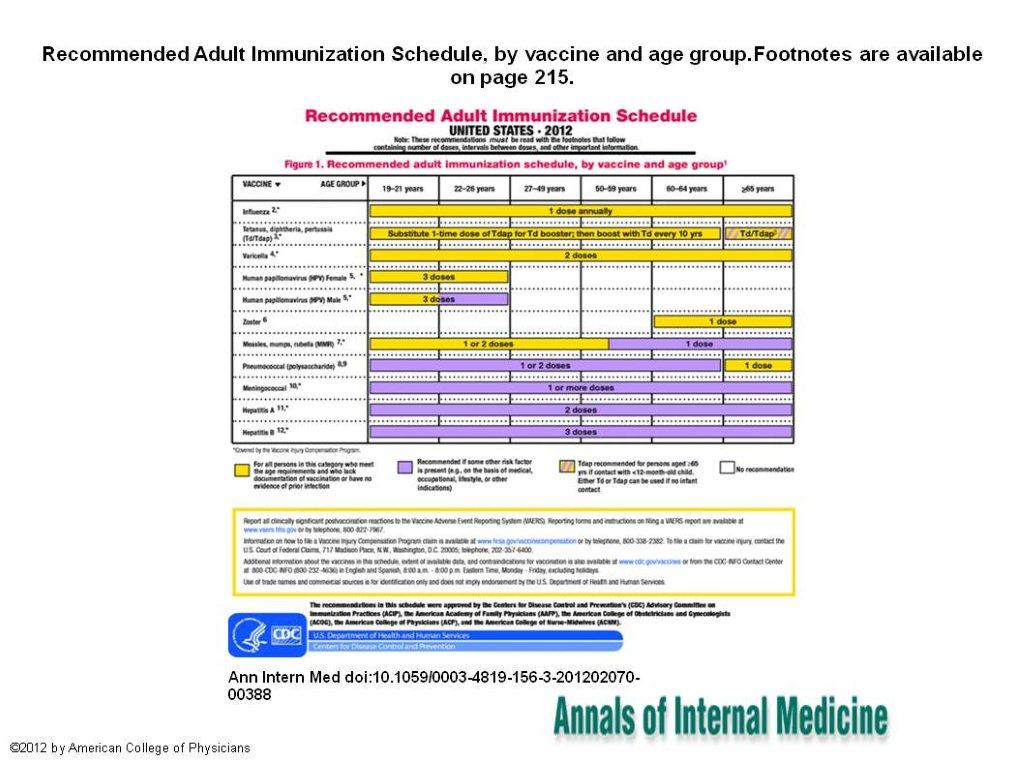
Adult Immunization Schedule: United States, 2012
Posted by: admin on: March 27, 2012
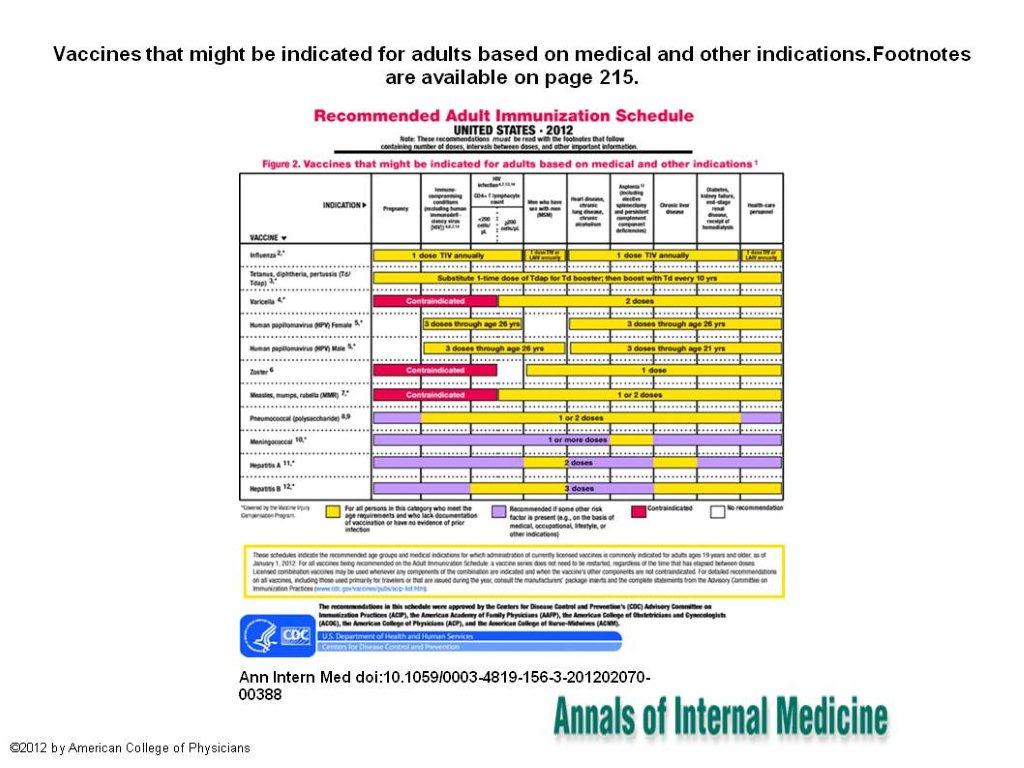
The Advisory Committee on Immunization Practices (ACIP) annually reviews the recommended Adult Immunization Schedule to ensure that the schedule reflects current recommendations for licensed vaccines.
-Team@CMHF
- In October 2011, ACIP approved the Adult Immunization Schedule for 2012, which includes several changes from 2011.
- A footnote directing readers to links for the full ACIP vaccine recommendations and where to find additional information on specific vaccine recommendations for travelers is now included.
- Changes to the footnote for the tetanus, diphtheria, acellular pertussis (Tdap) and tetanus, diphtheria (Td) vaccines were made to update recommendations.
- Tdap vaccine is recommended specifically for persons who are close contacts of infants younger than 12 months of age (for example, parents, grandparents, and child care providers) and who have not received Tdap previously.
- Before 2011, vaccination postpartum was preferred for women who had not had a previous adult Tdap dose.
- However, in 2011, ACIP recommended that pregnant women preferentially receive Tdap vaccination during later pregnancy (>20 weeks’ gestation). Other adults who are close contacts of children younger than 12 months of age continue to be recommended to receive a one-time dose of Tdap vaccine.
- Updates to the footnotes and figures were also made for the human papillomavirus (HPV) and hepatitis B vaccines based on recommendations made at the October 2011 ACIP meeting.
- The HPV vaccine recommendation has been updated to include routine vaccination of males aged 11 to 12 years, with catch-up vaccination recommended for males aged 13 to 21 years.
- HPV vaccine also is recommended for previously unvaccinated males aged 22 to 26 years who are immunocompromised, who test positive for HIV infection, or who have sex with men.
- ACIP also voted in October 2011 to recommend hepatitis B vaccine for adults younger than age 60 years who have diabetes, as soon as possible after diabetes is diagnosed.
- In addition, hepatitis B vaccination is recommended at the discretion of the treating clinician for adults with diabetes aged 60 years or older based on a patient’s likely need for assisted blood glucose monitoring, likelihood of acquiring hepatitis B, and likelihood of immune response to vaccination.
- A notation was included for the zoster vaccine to acknowledge that the vaccine was recently approved by the US Food and Drug Administration (FDA) for administration to persons 50 years of age and older; however, ACIP continues to recommend that vaccination begin at age 60 years.
- The influenza vaccine footnote was revised to specify age indications for the different licensed formulations of trivalent inactivated influenza vaccine (TIV).
- The footnote for the measles, mumps, rubella (MMR) vaccine was simplified to focus only on routine use of this vaccine in adults; information on use of the vaccine for outbreak control was removed. Readers are referred to the ACIP MMR recommendations and to the ACIP recommendations for the immunization of health-care personnel (HCP) regarding the use of MMR vaccine in outbreak settings. Additional information on the use of quadrivalent meningococcal conjugate vaccine (MCV4) and meningococcal polysaccharide vaccine (MPSV4) for specific age and risk groups was added.
- Minor clarifications also were made to the footnotes for HPV vaccine, varicella vaccine, and pneumococcal polysaccharide vaccine (PPSV).
Changes to the Schedule for 2012
- A new footnote, Additional information (footnote 1), has been added to the beginning of the footnotes.
- This footnote provides links to the full ACIP vaccine recommendations and information on travel requirements that may have been referred to previously in subsequent footnotes.
- The influenza vaccination footnote (footnote 2) was revised to clarify that all persons aged 6 months or older can receive TIV and that HCP who care for persons requiring a protected environment should receive TIV. Health-care personnel younger than 50 years who do not have a contraindication may receive either the live attenuated influenza vaccine or TIV. In addition, age indications for 2 recently licensed formulations of TIV were included. The link to additional information regarding influenza vaccination has been removed because a link now is provided in footnote 1.
- The HPV vaccination footnote (footnote 5) now clarifies that although HPV vaccination is not specifically recommended for HCP, they should receive the vaccine if they are in the recommended age group. This footnote was also changed to reflect the recommendation of the quadrivalent human papillomavirus (HPV4) vaccine for males aged 11 or 12 years and catch-up vaccination for males 13 to 21 years of age. Males aged 22 to 26 years may be vaccinated with HPV4 vaccine.
- The zoster vaccination footnote (footnote 6) now indicates that although zoster vaccination is not specifically recommended for HCP, they should receive the vaccine if they are in the recommended age group.
- This footnote also acknowledges that the vaccine is FDA-approved for use in persons aged 50 years or older; however, ACIP continues to recommend that vaccination begin at age 60 years.
- The PPSV vaccination footnote (footnote 8) has been revised to include additional examples of functional and anatomic asplenia. Language is included for persons with asymptomatic or symptomatic HIV infection and persons undergoing cancer chemotherapy or who are on other immunosuppressive therapy.
- The revaccination with PPSV footnote (footnote 9) has been revised to clarify guidance for those persons aged 65 years or older who had been vaccinated with PPSV23 before age 65 years and for whom at least 5 years has passed since their previous dose.
- The meningococcal vaccination footnote (footnote 10) has been revised to include military recruits in the group recommended to receive a single dose of meningococcal vaccine. The language about college students has been clarified to indicate that first-year college students up through age 21 years who are living in residence halls should be vaccinated if they have not received a dose on or after their 16th birthday.
- The hepatitis B vaccination footnote (footnote 12) has been revised to include persons with diabetes younger than age 60 years and persons aged 60 years or older based on need for assisted blood glucose monitoring.
Recommended Adult Immunization Schedule—United States, 2012
Influenza vaccination
Annual vaccination against influenza is recommended for all persons 6 months of age and older. Persons 6 months of age and older, including pregnant women, can receive the trivalent inactivated vaccine (TIV). Healthy, non-pregnant adults younger than age 50 years without high-risk medical conditions can receive either intranasally administered live, attenuated influenza vaccine (LAIV) (FluMist), or TIV. Health-care personnel who care for severely immunocompromised persons (ie, those who require care in a protected environment) should receive TIV rather than LAIV. Other persons should receive TIV.
The intramuscular or intradermal administered TIV are options for adults aged 18–64 years. Adults aged 65 years and older can receive the standard dose TIV or the high-dose TIV (Fluzone High-Dose).
Tetanus, diphtheria, and acellular pertussis (Td/Tdap) vaccination
Administer a one-time dose of Tdap to adults younger than age 65 years who have not received Tdap previously or for whom vaccine status is unknown to replace one of the 10-year Td boosters.
Tdap is specifically recommended for the following persons:
- pregnant women at more than 20 weeks’ gestation;
- adults, regardless of age, who are close contacts of infants younger than age 12 months (e.g., parents, grandparents, or child-care providers); and
- HCP.
Tdap can be administered regardless of interval since the most recent tetanus or diphtheria-containing vaccine.
Pregnant women not vaccinated during pregnancy should receive Tdap immediately postpartum.
Adults aged 65 years and older may receive Tdap.
Adults with unknown or incomplete history of completing a 3-dose primary vaccination series with Td-containing vaccines should begin or complete a primary vaccination series. Tdap should be substituted for a single dose of Td in the vaccination series with Tdap preferred as the first dose.
For unvaccinated adults, administer the first 2 doses at least 4 weeks apart and the third dose 6–12 months after the second.
If incompletely vaccinated (ie, less than 3 doses), administer remaining doses.
Varicella vaccination
All adults without evidence of immunity to varicella should receive 2 doses of single-antigen varicella vaccine or a second dose if they have received only 1 dose.
Special consideration for vaccination should be given to those who:
- Have close contact with persons at high risk for severe disease (eg, HCP and family contacts of persons with immunocompromising conditions); or
- Are at high risk for exposure or transmission (eg, teachers; child-care employees; residents and staff members of institutional settings, including correctional institutions; college students; military personnel; adolescents and adults living in households with children; non pregnant women of childbearing age; and international travelers).
Pregnant women should be assessed for evidence of varicella immunity. Women who do not have evidence of immunity should receive the first dose of varicella vaccine upon completion or termination of pregnancy and before discharge from the health-care facility. The second dose should be administered 4–8 weeks after the first dose.
Evidence of immunity to varicella in adults includes any of the following:
- documentation of 2 doses of varicella vaccine at least 4 weeks apart;
- US born before 1980 (although for HCP and pregnant women, birth before 1980 should not be considered evidence of immunity);
- history of varicella based on diagnosis or verification of varicella by a health-care provider (for a patient reporting a history of or having an atypical case, a mild case, or both, health-care providers should seek either an epidemiologic link to a typical varicella case or to a laboratory-confirmed case or evidence of laboratory confirmation, if it was performed at the time of acute disease);
- history of herpes zoster based on diagnosis or verification of herpes zoster by a health-care provider; or
- laboratory evidence of immunity or laboratory confirmation of disease.
Human papillomavirus (HPV) vaccination
Two vaccines are licensed for use in females, bivalent HPV vaccine (HPV2) and quadrivalent HPV vaccine (HPV4), and one HPV vaccine for use in males (HPV4).
For females, either HPV4 or HPV2 is recommended in a 3-dose series for routine vaccination at 11 or 12 years of age, and for those aged 13–26 years, if not previously vaccinated.
For males, HPV4 is recommended in a 3-dose series for routine vaccination at age 11 or 12 years and for those aged 13–21 years, if not previously vaccinated. Males aged 22–26 years may be vaccinated.
HPV vaccines are not live vaccines and can be administered to persons who are immunocompromised as a result of infection (including HIV infection), disease, or medications. Vaccine is recommended for immunocompromised persons through age 26 years who did not receive any or all doses when they were younger. The immune response and vaccine efficacy might be less than that in immunocompetent persons.
Men who have sex with men (MSM) may especially benefit from vaccination to prevent condyloma and anal cancer. HPV4 is recommended for MSM through age 26 years who did not get any or all doses when they were younger.
Ideally, vaccine should be administered before potential exposure to HPV through sexual activity; however, persons who are sexually active should still be vaccinated consistent with age-based recommendations. HPV vaccine can be administered to persons with a history of genital warts, abnormal Papanicolaou test results, or positive HPV DNA test results.
A complete series for either HPV4 or HPV2 consists of 3 doses. The second dose should be administered 1–2 months after the first dose; the third dose should be administered 6 months after the first dose (at least 24 weeks after the first dose).
Although HPV vaccination is not specifically recommended for HCP based on their occupation, they should receive the HPV vaccine if they are in the recommended age group.
Zoster vaccination
A single dose of zoster vaccine is recommended for adults aged 60 years and older regardless of whether they report a prior episode of herpes zoster. Although the vaccine is licensed by the US Food and Drug Administration for use among and can be administered to persons aged 50 years and older, ACIP recommends that vaccination begins at age 60 years.
Persons with chronic medical conditions may be vaccinated unless their condition constitutes a contraindication, such as pregnancy or severe immunodeficiency.
Although zoster vaccination is not specifically recommended for HCP, they should receive the vaccine if they are in the recommended age group.
Measles, mumps, rubella (MMR) vaccination
Adults born before 1957 generally are considered immune to measles and mumps. All adults born in 1957 or later should have documentation of 1 or more doses of MMR vaccine unless they have a medical contraindication to the vaccine, laboratory evidence of immunity to each of the 3 diseases, or documentation of provider-diagnosed measles or mumps disease. For rubella, documentation of provider-diagnosed disease is not considered acceptable evidence of immunity.
Measles component:
A routine second dose of MMR vaccine, administered a minimum of 28 days after the first dose, is recommended for adults who:
are students in postsecondary educational institutions;
work in a health-care facility; or
plan to travel internationally.
Persons who received inactivated (killed) measles vaccine or measles vaccine of unknown type from 1963 to 1967 should be revaccinated with 2 doses of MMR vaccine.
Mumps component:
A routine second dose of MMR vaccine, administered a minimum of 28 days after the first dose, is recommended for adults who:
are students in postsecondary educational institutions;
work in a health-care facility; or
plan to travel internationally.
Persons vaccinated before 1979 with either killed mumps vaccine or mumps vaccine of unknown type who are at high risk for mumps infection (e.g., persons who are working in a health-care facility) should be considered for revaccination with 2 doses of MMR vaccine.
Rubella component:
For women of childbearing age, regardless of birth year, rubella immunity should be determined. If there is no evidence of immunity, women who are not pregnant should be vaccinated. Pregnant women who do not have evidence of immunity should receive MMR vaccine upon completion or termination of pregnancy and before discharge from the health-care facility.
HCP born before 1957:
For unvaccinated HCP born before 1957 who lack laboratory evidence of measles, mumps, and/or rubella immunity or laboratory confirmation of disease, health-care facilities should consider routinely vaccinating personnel with 2 doses of MMR vaccine at the appropriate interval for measles and mumps or 1 dose of MMR vaccine for rubella.
Pneumococcal polysaccharide (PPSV) vaccination
Vaccinate all persons with the following indications:
aged 65 years and older without a history of PPSV vaccination;
adults younger than age 65 years with chronic lung disease (including chronic obstructive pulmonary disease, emphysema, and asthma); chronic cardiovascular diseases; diabetes mellitus; chronic liver disease (including cirrhosis); alcoholism; cochlear implants; cerebrospinal fluid leaks; immunocompromising conditions; and functional or anatomic asplenia (eg, sickle cell disease and other hemoglobinopathies, congenital or acquired asplenia, splenic dysfunction, or splenectomy [if elective splenectomy is planned, vaccinate at least 2 weeks before surgery]);
residents of nursing homes or long-term care facilities; and
adults who smoke cigarettes.
Persons with asymptomatic or symptomatic HIV infection should be vaccinated as soon as possible after their diagnosis.
When cancer chemotherapy or other immunosuppressive therapy is being considered, the interval between vaccination and initiation of immunosuppressive therapy should be at least 2 weeks. Vaccination during chemotherapy or radiation therapy should be avoided.
Revaccination with PPSV
One-time revaccination 5 years after the first dose is recommended for persons aged 19–64 years of age with chronic renal failure or nephrotic syndrome; functional or anatomic asplenia (eg, sickle cell disease or splenectomy); and immunocompromising conditions.
Persons who received PPSV before age 65 years for any indication should receive another dose of the vaccine at age 65 years or later if at least 5 years have passed since their previous dose.
No further doses are needed for persons vaccinated with PPSV at or after age 65 years.
Meningococcal vaccination
Administer 2 doses of meningococcal conjugate vaccine quadrivalent (MCV4) at least 2 months apart to adults with functional asplenia or persistent complement component deficiencies.
HIV-infected persons who are vaccinated should also receive 2 doses.
Administer a single dose of meningococcal vaccine to microbiologists routinely exposed to isolates of Neisseria meningitidis, military recruits, and persons who travel to or live in countries in which meningococcal disease is hyperendemic or epidemic.
First-year college students up through age 21 years who are living in residence halls should be vaccinated if they have not received a dose on or after their 16th birthday.
MCV4 is preferred for adults with any of the preceding indications who are aged 55 years and younger; meningococcal polysaccharide vaccine (MPSV4) is preferred for adults aged 56 years and older.
Revaccination with MCV4 every 5 years is recommended for adults previously vaccinated with MCV4 or MPSV4 who remain at increased risk for infection (e.g., adults with anatomic or functional asplenia or persistent complement component deficiencies).
Hepatitis A vaccination
Vaccinate any person seeking protection from hepatitis A virus (HAV) infection and persons with any of the following indications:
- MSM and persons who use injection drugs;
- persons working with HAV-infected primates or with HAV in a research laboratory setting;
- persons with chronic liver disease and persons who receive clotting factor concentrates;
- persons traveling to or working in countries that have high or intermediate endemicity of hepatitis A; and
- Unvaccinated persons who anticipate close personal contact (e.g., household or regular babysitting) with an international adoptee during the first 60 days after arrival in the United States from a country with high or intermediate endemicity. (See footnote 1 for more information on travel recommendations.) The first dose of the 2-dose hepatitis A vaccine series should be administered as soon as adoption is planned, ideally 2 or more weeks before the arrival of the adoptee.
Single-antigen vaccine formulations should be administered in a 2-dose schedule at either 0 and 6–12 months (Havrix), or 0 and 6–18 months (Vaqta). If the combined hepatitis A and hepatitis B vaccine (Twinrix) is used, administer 3 doses at 0, 1, and 6 months; alternatively, a 4-dose schedule may be used, administered on days 0, 7, and 21–30 followed by a booster dose at month 12.
Hepatitis B vaccination
Vaccinate persons with any of the following indications and any person seeking protection from hepatitis B virus (HBV) infection.
- sexually active persons who are not in a long-term, mutually monogamous relationship (e.g., persons with more than 1 sex partner during the previous 6 months); persons seeking evaluation or treatment for a sexually transmitted disease (STD); current or recent injection-drug users; and MSM;
- HCP and public-safety workers who are exposed to blood or other potentially infectious body fluids;
- persons with diabetes younger than 60 years as soon as feasible after diagnosis; persons with diabetes who are aged 60 years or older at the discretion of the treating clinician based on increased need for assisted blood glucose monitoring in long-term care facilities, likelihood of acquiring hepatitis B infection, its complications, or chronic sequelae, and likelihood of immune response to vaccination;
- Persons with end-stage renal disease, including patients receiving hemodialysis; persons with HIV infection; and persons with chronic liver disease;
- household contacts and sex partners of persons with chronic HBV infection; clients and staff members of institutions for persons with developmental disabilities; and international travelers to countries with high or intermediate prevalence of chronic HBV infection; and
- all adults in the following settings: STD treatment facilities; HIV testing and treatment facilities; facilities providing drug-abuse treatment and prevention services; health-care settings targeting services to injection-drug users or MSM; correctional facilities; end-stage renal disease programs and facilities for chronic hemodialysis patients; and institutions and nonresidential day-care facilities for persons with developmental disabilities.
Administer missing doses to complete a 3-dose series of hepatitis B vaccine to those persons not vaccinated or not completely vaccinated. The second dose should be administered 1 month after the first dose; the third dose should be given at least 2 months after the second dose (and at least 4 months after the first dose). If the combined hepatitis A and hepatitis B vaccine (Twinrix) is used, give 3 doses at 0, 1, and 6 months; alternatively, a 4-dose Twinrix schedule, administered on days 0, 7, and 21–30 followed by a booster dose at month 12 may be used.
Adult patients receiving hemodialysis or with other immunocompromising conditions should receive 1 dose of 40 mcg/mL (Recombivax HB) administered on a 3-dose schedule or 2 doses of 20 mcg/mL (Engerix-B) administered simultaneously on a 4-dose schedule at 0, 1, 2, and 6 months.
Selected conditions for which Haemophilus influenzae type B (Hib) vaccine may be used
One dose of Hib vaccine should be considered for persons who have sickle cell disease, leukemia, or HIV infection, or who have anatomic or functional asplenia if they have not previously received Hib vaccine.
Immunocompromising conditions
Inactivated vaccines generally are acceptable (eg, pneumococcal, meningococcal, and influenza (inactivated influenza vaccine) and live vaccines generally are avoided in persons with immune deficiencies or immunocompromising conditions.
For further reading log on to
http://www.annals.org/content/early/2012/01/30/0003-4819-156-3-201202070-00388.full
Search
- drchasrani: Difficult to get such a data, authenticated at that. Try Times of India online library
- rakesh pore: hi, where can i get genuine information about "10 most common drugs sold in india?" i want it for a local project
- nilesh dutta: sir, Plz give detail about MBA Sports Management Thanks and Regards


Leave a Reply